|
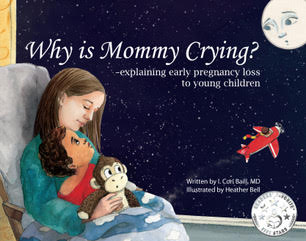
By: Maria Servold EPLA Editor Many parents who experience early pregnancy loss have found themselves at adrift when it comes to explaining the miscarriage to any living children they may already have. They may wonder: How do I explain that the baby isn’t going to be born? What if they ask where it went? Will I cause them pain by explaining it? One OB-GYN and mother has written a picture book that gives parents the tools to help explain early loss to children. “Why is Mommy Crying?” by I. Cori Baill, M.D., is a beautiful picture book about a boy named Max who sees his mommy crying and wants to know why. With simple, graceful text and beautiful pictures, Baill and illustrator Heather Bell created a wonderful book that can serve as a resource and jumping-off point for discussing miscarriage with children. Baill spent many years in practice as an OB-GYN and now teaches at the University of Central Florida College of Medicine. After suffering a miscarriage early in her medical career, Baill said she found herself looking for resources to help her explain the loss to the two small children she already had. “I was very surprised at the lack of resources, starting with my religion, which said there was no ceremony, there was no prayer, there was no ritual,” she said. I was really surprised that there was not much out there to help me explain [miscarriage] to my children.” Afterward, she said, she had a “germ of an idea” about a children’s book that could help explain early pregnancy loss. Baill said she watched and waited, certain someone would write and publish such a book. “I had this idea for a children’s book that I thought was really needed,” she said. “I didn’t think I was the right person to write it. I didn’t think I was an expert. I kept my eye out for the book; kept looking for someone to write it.” But no one did. So, eventually, Baill wrote it herself. In addition to helping explain miscarriage itself to children, Baill said she hopes the book can serve as a springboard for discussion among parents and their children. In the back of the book, she provides a list of resources for helping children through grief, for example. The paperback book is available for purchase online, and would make a beautiful addition to any family’s library. We also encourage our readers to consider purchasing it for their local library or pregnancy resource center. Below are several excerpts of my video interview with Dr. Baill. Dr. Baill introduces herself: What prompted you to write this book? Finding and working with illustrator Heather Bell: Why is miscarriage important to discuss? Thank you so much to Dr. Baill for her time, and for writing a beautiful book that will help provide support to families suffering early pregnancy loss.
Maria Servold is an Editor at the EPLA, Assistant Director of the Herbert H. Dow II Program in American Journalism, and Lecturer in Journalism at Hillsdale College.
1 Comment
By Emily Graham  Pregnancy loss is one of the most gut-wrenching tragedies that can strike a family. Losing a child due to a miscarriage or stillbirth can be just as devastating as losing an older child, and it’s very common to develop serious depression and anxiety in the subsequent weeks and months.
It’s important to know that it’s okay to feel sad. Don’t let anyone tell you how to grieve. A loss like this - one so personal - is going to take time to fully heal. Having said that, it’s also important that you know that there are ways to help you manage your depression. The Early Pregnancy Loss Association hopes this guide will offer you some hope and support during this unimaginable time. Know when ‘healthy’ grief turns into something worse There’s no set timeline for dealing with a loss of this caliber. Every parent reacts differently, with some pushing through and surfacing in a good emotional place faster than others. Nobody can tell you how you should feel, but you should know that grief of this nature tends to “move,” according to Postpartum Progress. “‘Healthy’ grief moves, but sometimes it can develop into relentless depression that requires more specific treatment. Many moms will experience depression that includes feelings of guilt, shame, self-doubt, and sometimes suicidal ideation. Regaining a sense of self, hope, and trust is important to one’s healing after a loss such as this,” says the blog. If you find yourself “stuck” in a rut of depression for an extended period of time, it may be a signal to seek professional help. Don’t be afraid to reach out and get out There are no rules for this. Nobody says you have to struggle with the pain alone. When dealing with depression, reaching out to friends and family for support can be a great way to start to heal. Try to get out and do things that make you feel happy - even if it’s hard. The loss of a child through miscarriage is not your fault, and there’s no need to punish yourself in solitude. Boost your body and brain for better mental health Depression and anxiety start in the brain, but develop a life of their own after a while and begin to negatively affect every part of your body. If you find yourself suffering from depression, it will help to take the time to take care of your mind and body. For your mind, turn to a practice like meditation, which has been proven to help reduce the effects of stress and anxiety. You can even create a “solitude space” in your home dedicated to meditation so you can get the most benefits from this practice. Make sure the area you choose is away from the everyday hustle-and-bustle of your household, and resist having distractions like electronic devices. Sometimes indulgence is one way to deal with stress and anxiety, but it can have long-term effects if ignored. Are you overeating? Or perhaps even drinking more than usual? Look at what you’re eating and drinking and see where you can make improvements. A poor diet gives your brain and body the wrong type of fuel, and it’s hard to overcome depression when your brain is running on processed foods. Exercise is important too, as it can help you clear your head and release chemicals that trigger your brain’s happy centers. Physical activity has a way of forcing the brain to refocus, and through repeated efforts you are likely to see a noticeable improvement in how you feel. Getting a good night’s sleep is also important and you should for at least 8 hours a night. If you are having trouble sleeping, physical activity should help, but it’s also good to remove distractions from your bedroom like TVs, phones, or tablets. Additionally, a light yoga flow is a great way to prep your mind and body for a good night’s sleep. Turn to other companionship Oftentimes turning to family and friends is not enough, or perhaps they don’t understand how to talk about what you are going through. When battling severe depression, enlist the help of a counselor and spend time with a support group. You do not have to weather this storm alone, and being around people who can help you through your grief will prevent feelings of isolation. Do be gentle with yourself throughout this process. You are not running a race, and there’s no reason to add extra pressure. Time does bring healing, but when you are in the thick of depression, it’s impossible to pinpoint when or how long that will be. In the long run, being good to yourself and taking extra care will make navigating the difficult road of loss more manageable. For more supportive resources, visit the Early Pregnancy Loss Association website. Photo Credit: Pixabay.com By Heather Heritage M.A. The first trimester of my 4th pregnancy was rough. Not only was I exhausted with two young children and working full time, I had severe nausea and dehydration problems - so severe I ended up in the ER on more than one occasion. Most of the questions the ER staff askedwere perfunctory, trying to piece together my condition and background information to get a clear picture for treatment. But when a young physician’s assistant commented on my gestational and pregnancy history, imagine my shock when she bluntly stated, “oh, I see you had an abortion last year.” I had a miscarriage six months prior to that ER visit, and I knew that medical terminology technically classifies any pregnancy loss as an abortion of some sort. But knowing this didn't really take the sting out of her unempathetic words. In the end, I got the fluids I needed and went on my way, but couldn't shake the annoyance of the term “abortion” that was used to describe my miscarriage. Using the word abortion when referencing a miscarriage can be hurtful and alienate the very patients a health care provider (HCP) is trying to build rapport with and treat, even if it is “proper” medical terminology. In the area of early pregnancy loss (miscarriage), there are large inconsistencies in how providers communicate to mothers about the loss they are experiencing, which can result in a lack of thorough treatment and care for these vulnerable patients. A 2019 study explored early pregnancy loss and gaps in the physical, cognitive, and emotional treatment of patients. Using those criteria as a framework, I offer considerations in a triangle of treatment plan for health care providers to use with their patients who go through pregnancy loss. Physical Care The first, and most pertinent point in the triangle, is caring for the physical needs of a patient. In 2019, the American Pregnancy Association reported that one in five women with recognized pregnancies end in miscarriage, making it a fairly common experience. Because of their often abrupt and sudden nature, many women seek help at the emergency room. However, there are significant gaps of care for patients, specifically in the ER, regarding communication, diagnostic testing and follow up instruction. Delays in or failure to complete diagnostic tests occur, specifically with blood work and ultrasounds. In many situations, mothers have left a treatment center without knowing if they had lost their baby, what to expect, and without full comprehension of their condition. Even if the tests are completed, often there are long wait times for results – which could mean leaving a patient for hours, worrying and stressing that their pregnancy is ending. Much of these wait times are due to logistical barriers; however, those delays or obstructions should be communicated and clarified to the patient. There is another gap in treatment: scheduling follow-up visits, which are important for incomplete miscarriages, and cognitive and emotional healing. Often these follow-ups are never discussed or mentioned with a patient. Tips for health care providers caring for the physical point in the triangle of treatment include:
Cognitive Care The second point in the triangle of treatment focuses on cognitive care; specifically, using common terminology, and being able to explain what is happening and give thorough information. There is a need for common language when it comes to early pregnancy loss. Early pregnancy loss means any fetal loss at or before 13 weeks of gestation. This is also referred to as: miscarriage, fetal death, perinatal loss, spontaneous abortion, missed abortion, etc. HCPs need to understand that language and terminology have different meanings to different people, and HCPs need to be aware of this when communicating with their patients. A good tip in getting the terminology right is to use mirroring terms. For example, if a patient uses the term “baby” or “child,” an HCP should mirror their language by referring to the loss in matching terms. Patients also need more in‐depth explanation and communication on the causes of miscarriage, frequency of miscarriage, and their diagnostic test results. HCPs would do well to remember that this is a painful and emotional process for the patient. If a patient is being told the pregnancy is over; all of the hopes and dreams for a viable baby come to a glaring and final halt in that moment. They deserve explanation and information, both in verbal and written communication. Patients and their personal caretakers have said they want more information about physical complications, current treatment, resumption of menstruation, future pregnancies, and emotional health and healing. Tips for HCPs in the cognitive point in the triangle of treatment include:
Emotional Care The third point in the triangle of treatment stresses emotional care for miscarrying patients. There are many opportunities for HCPs to communicate with empathy and offer comfort in bereavement support. Mothers are experiencing shock, sadness, worry, guilt, helplessness, and yet often, there is little empathy provided. In addition, in an ER, there is little privacy, space, and time to process the diagnosis or for providers to simply listen to a patient. More could be done in allowing for the opportunity for mothers to express their grief and emotions. Tips for HCPs in the emotional point in the triangle of treatment include: 1. Encourage patient to talk and discuss their feelings. Give comfort specifically to alleviate feelings of guilt. 2. Encourage sharing of their experience when they are ready. Recommend social groups, websites, blogs, alternative therapies like poetry/art, etc. as it helps in the grieving process. 3. Encourage patients to read prominent stories of women in the public eye who have had a common experience, for example, Chrissy Teigen or Meghan, The Duchess of Sussex. This helps normalize the experience, and patients can find hope in common loss. 4. Understand, practice, and deliver bereavement support in the form of companion care. Dr. Wolfelt, Founder and Director of the Center for Loss and Life Transition defines companion care as:
5. For providers in managerial roles: Consider the use of doulas who specialize in pregnancy loss. A doula is a non-medical person who supports a woman during labor and birth, pregnancy loss, bereavement, and postpartum healing, and are trained to provide one-on-one care, physical comfort, companion care and emotional support. There is often funding via grants or programs that can bring doula care into a treatment center. Caring for the Whole Person Early pregnancy loss is a highly emotional and nuanced situation for each individual. Health care providers are inconsistent in how they communicate to and support mothers going through this sorrow. Understanding these implications would help them treat their patients more effectively, using a triangle of treatment to meet the physical, cognitive and emotional needs of these patients. We’ve all been in highly emotional situations and know that compassion and empathy can go a long way in humanizing the situation. HCPs who implement these suggestions could have a positive impact on grieving mothers for years to come. Heather Heritage is an Assistant Professor of Communication at Cedarville University.
By: Brian Sinischo, M.D. Experiencing loss is painful, both physically and mentally. As an expectant mother, partner, family member, friend, or health care provider, we all face this loss from our own perspective. I remember the first time I diagnosed a fetal demise by ultrasound. I was in my first year of residency. I was working on the OB floor in Saginaw, Michigan and one of the nurses came to me and asked me to find a baby’s heart tone as she couldn’t find it with the doppler. I didn’t have enough experience to even get anxious about this ultrasound. I took the machine into the room, gelled up the patient’s abdomen, and used the abdominal probe to assess the heartbeat. The baby was 34 weeks along, and it should take four seconds to find, but when I got in the right position there was no cardiac activity. I didn’t realize I changed, but my expression must have shown my thoughts. The mother went into protection mode and started asking this young doctor some hard questions. "What’s wrong? Why is your face like that? Where is my doctor?" Very soon, tears started to come. I kept my composure and explained what I was seeing. I showed her the heart and showed her how there was no movement when there should have been. Then my tears started… I remember wanting to make it all better, but I couldn’t. The program I trained in allowed us to follow patients through their time with us, giving us the chance to learn and watch all of the stages of birth. I will never forget this induction and helping deliver this baby that looked so perfect, and watching as the family grieved on what should have been a joyous day. I left that delivery and cried too. I spent a lot of time listening to this family and how they worked through their grief. It was educational and, honestly, some of the hardest medicine I have had to learn. Much of medicine, I have learned, has nothing to do with drugs or procedures. I feel in many ways I live in two worlds. One, the medical world of terminology, definition, safe practice, protocol, medication, and sterility. The other world is heart-related, compassionate, and not linear. Traditionally, physicians are trained to separate the two worlds, probably so the practitioner can function, despite the tragedy unfolding in front of them. But I’m learning how to blend the two. Here are a few things I have learned to do: 1) Offer ultrasounds. (I drag the ultrasound machine all over my office and the hospital to show patients exactly what is going on inside before any procedure or induction or decision needs to be made.) 2) Attempt to keep medical jargon to a minimum and repeat myself. Often when trauma occurs it is hard for a person to remember what was said and comprehending new information is hard. 3) Allow time. Patients need time to process and make decisions. There are times when patients come to the office three or more times before they make a decision on how to move forward. There is a fine line to be walked when informing patients of risks associated with loss. Watching and waiting is almost always an option but comes with risk of infection, hemorrhage, and sometimes worsened mental anguish. There is no one right answer when deciding how to treat the loss of a baby. It often feels like we are forced to make a decision in an impossible situation, as many families are in a devastated mental state. I have also learned to never take it personally. I have been hit, screamed at, kicked, cried and vomited on, hugged, and prayed with. This process is tumultuous. When someone is going through their worst day, I strive to be calm, compassionate, consistent, and know that it’s okay to cry. Some may consider it unprofessional; I consider it human. If you have gone through the loss of a baby, I’m deeply sorry. I hope compassion is what met you, and I apologize if it was not. We learn as we go and sometimes as medical professionals we learn from our current situation. Most physicians and medical professionals I have had the privilege to work with and desire to serve, understand, and help. During trauma, many emotions are involved and, unfortunately, like my facial expressions from the above episode, are mistakenly shared. In attempted grace, I hope to serve Hillsdale well and grow in the amazing teams with whom I get to serve. Brian Sinischo is a OB/GYN at Hillsdale Hospital.
By: Sarah Gregory EPLA Vice President
In every community around the world, families experiencing miscarriage need support from their community networks. Churches and other religious communities play an important role in bearing the burden of grief. How can faith communities help in the midst of the invisible grief of miscarriage? Rituals- Funerals, memorials, and worship Many families need the sense of closure that grief rituals like funerals provide. Reach out to your local funeral home to find out information about miscarriage burial possibilities. Some families do not have a physical body to bury, so consider potential alternatives like a memorial service, memorial garden, or private ritual for closure. Many denominations already have child loss and miscarriage worship outlines in their established worship resources. If you are affiliated with a denomination, look into the established worship rituals for services for infant death and grieving families. Pastors and chaplains can also prepare with established prayers, scripture, and music that particularly fit the burden of miscarriage to share with grieving parents in private moments. Provide a Meal It’s good practice to ask first to be sure the family wants the meal support. Don't be afraid to use your network to provide tangible support while a family wades through the logistical coordination, health decisions, confusion, and emotional trauma a miscarriage creates. Know your Resources Organizations like the Early Pregnancy Loss Association provide educational materials and other resources to women suffering from a miscarriage. Download our educational resources from our website. Local community groups also provide support. A quick search online can start you in the right direction. You can also find out what organizations may already exist by talking to healthcare providers, counselors, or community leaders. Listen, Affirm, and Remember Perhaps the most crucial piece of supporting a family through miscarriage is to listen to the grief and affirm their loss. Families experience long lasting pain that is invisible to most people. Affirm that their grief is real. Check in on the family during the anniversary of the miscarriage or due date. Simply remembering the loss will instill the sense that they are not alone. Faith communities provide emotional and spiritual support during times of grief. Be sure to deploy the networks and systems reserved for moments of trauma and pain at the pace and rate at which the family experiencing loss feels most comfortable. Faith communities can and do provide important healing, support, and hope. Worship Resources: Luthern “Martin Luther’s Comfort for Women Who have had a Miscarriage” https://blogs.lcms.org/2016/miscarriage-comfort-in-a-time-of-loss/ Non-Denominational http://www.preachitteachit.org/articles/detail/helping-her-grieve-how-to-have-a-funeral-for-miscarried-or-aborted-babies/ Othodox Church in America https://oca.org/orthodoxy/prayers/service-after-a-miscarriage-or-stillbirth United States Conference of Catholic Bishops http://www.usccb.org/prayer-and-worship/bereavement-and-funerals/blessing-of-parents-after-a-miscarriage-or-stillbirth.cfm United Methodist https://www.umcdiscipleship.org/resources/ministry-immediately-following-death Sarah Gregory is a Christian Education freelance writer, consultant, and musician. Sarah lives in St. Louis with her husband Kaleb and her son Cecil. Note: This post was originally written by Joy for the purposes of Henry Ford Allegiance Health in Jackson, Michigan. It is being published with permission from the author. By: Joy Sterrett, RN. You may never see your child play t-ball, dance ballet, or ride a bike, but you are still a mom. You are still a dad. You may never get to walk your daughter down the aisle, but you are still a dad. You may never see your dreams for your precious child come to fruition, but you are still a parent. I wanted to reassure parents who have experienced a loss that they have every right to celebrate being a mother and a father. Regardless if the loss was from a miscarriage, full-term baby, or even a young child, a loss does not strip away the parent title. I encourage everyone who has experienced a loss to think of creative ways to commemorate their baby’s life. Here are some ideas:
Those who’ve experienced a loss can feel very isolated in their grief. I want to encourage you to look around you. See all of the other families surrounding you. Remember you are never alone. There are many who have walked a similar path, and there are those who will hold your hand through your journey of grief. Don’t let today be the last time that you celebrate your baby’s life. And never forget you are still a mom. You are still a dad. Joy Sterret is the Perinatal Beareavement Coordinator at Henry Ford Health Services in Jackson, Michigan.
By: Rose Carlson, Program Director of Share Pregnancy & Infant Loss Support Like many of you reading this post, from the moment I saw my first positive pregnancy test, my life changed forever. When my first two pregnancies ended abruptly at 11 and 6 weeks, I was truly unprepared for the intensity of my feelings and the seeming lack of concern from my friends and family. My heart was completely shattered, not only by the losses of my babies but also by the reactions of my loved ones. Nearly two years after my second miscarriage, I gave birth to my son Brandon, who will soon be 28. I breathed an enormous sigh of relief and assumed my experience with the heartbreak of loss was over. That was not to be, and I went on to have two more miscarriages, at 13 and 10 weeks. I was devastated. And back in those days, in the late ’80s and early ’90s, support for women like me was practically non-existent. Nothing I received back then was anything close to what this brokenhearted mom needed. I received no flowers, sympathy cards, or meals after surgeries. No mementos to fondly remind me of my babies. No bereavement information from the medical community. No support groups to help me feel less alone. Most distressing, I received no acknowledgement that these babies were great losses to me. Rather than the loving care I desperately wanted and needed, I instead received hurtful words such as: “These things happen for a reason,” “There was probably something wrong with ‘it.’” “At this stage, it’s not a real baby.” “Be grateful it happened early, before you got attached.” “Move on and have FUN trying again!” As anyone who has experienced an early pregnancy loss and heard similar sentiments knows absolutely none of those words were helpful or comforting. But sadly, that was all I was hearing, and without any other support, I believed my feelings of grief were unnatural. I did (or, I thought I did) what was encouraged and expected of me: I pushed my emotions aside. I “moved on” and had three more children. I was a busy stay-at-home mom who forced myself to quickly dismiss any thoughts of those four babies whenever they made their way into my heart. It wasn’t until I began volunteering at Share, nine years after my last loss, that I learned my grief was not “unnatural” at all; I received permission to acknowledge the confusing feelings I had pushed aside for so long. One of the most profound things I felt when I started volunteering at Share was, “Wow, I wasn’t crazy back then!” It was eye-opening, both the acknowledgement of my feelings as well as the support I came to receive. As I met and got to know other grieving parents and read articles in the Share newsletter, I realized that compassionate support truly can make a difference, and I knew what a positive impact that kind of support would have meant to me.
“Indeed, it is a uniquely powerful experience to be surrounded by other people who have experienced the death of a child.” ~Carol McMurrich I love quotes, and I especially love this one, as it perfectly sums up my feelings about the value of the support bereaved parents receive from others who have also experienced a miscarriage or other pregnancy loss. There is a common misconception that those who lose a baby, especially early in pregnancy, will not grieve as deeply as someone who loses an older child or a full-term baby. This is not necessarily the case. Many parents who experience early pregnancy loss often are in great need of support yet, like me, are unable to find it among their family and friends. Attending a support group, either online or face-to-face, can fill this void and provide meaningful, healing support. Being with others who are grieving and seeking a path of healing after a miscarriage can help parents cope, as well as provide hope that they too can survive this loss. A support community offers bereaved parents safety and acceptance as they share their hearts and stories among others who understand and are walking a similar journey. Support groups offer additional positive effects on healing, too. Support groups can:
At Share, we have learned that it can be uncomfortable, even downright scary, to walk into a support group meeting for the first time. Parents may feel uncertain of what to expect or even of what they might need, but we have seen firsthand the value of shared support. Keep in mind that peer support groups are not meant to be “therapy,” which can feel intimidating. A support group is simply meant to be a safe, loving place where grieving parents can talk about their baby and connect with others in a similar situation. Thankfully, there is more support today than ever before, through support groups both in our communities and online. Because I did not have the opportunities for support that are available today, I have made it my personal mission to help parents find the support that leads them forward in their healing journey, and memorialize their baby. That is how I honor and remember the four babies who touched my heart in countless ways. Rose Carlson is the Program Director of Share Pregnancy & Infant Loss Support By: Kathy Petersen I found out I was pregnant with my second baby when my oldest was only 9 months old. We were pretty overwhelmed, but excited, and went to the first OB appointment at 10 weeks. We didn’t hear a heartbeat. Our physician gave us encouragement that it was still early, position and size of the baby could affect the ability to hear the heartbeat, and said, “we’ll just check next time.” Four weeks went by and at my 14-week appointment, there was still no heartbeat. My OB sent me for an ultrasound to confirm, and while I was no ultrasound expert, there was no movement, no heartbeat, and no life on the screen. I went home sad, disappointed, and a little unsure of what I was supposed to do or expect. This new information didn’t just change that day; it changed that week, the next nine months, the next 18 years, the rest of my life. But 20 years later and as a mother of eight, I have come to realize that every experience in our journey of motherhood, every joy and every suffering, changes us. We grow, we learn, we adapt, we cope. Every experience, my miscarriage included, has shaped who I am as a mother. I didn’t expect that my miscarriage would shape who I am as a nurse as well. As a labor and delivery nurse for 20 years, I have been at the side of many women who have had a pregnancy loss. I have cried with them, taken pictures for them, and just sat at their bedsides. Women who experience a pregnancy loss need postpartum care: physical needs like Tylenol and Motrin, pads, and fluids, but also emotional needs like visits, meals, and friends. People know how to celebrate babies, but most people are uncomfortable supporting others during a miscarriage. It’s not easy, but those of us who have had miscarriages should be first in line to be present to others who have sadly joined us. Groups like the Early Pregnancy Loss Association are a great support and are helping to bring the topic of early pregnancy loss into the light so that no woman feels alone. Women might also experience something similar to postpartum depression after a miscarriage, though there is debate as to whether it is actually postpartum depression or not. A drop in hormones coupled with the emotional event of losing a baby can trigger extreme anxiety and other mental health issues.
Many women may think that because the pregnancy ended early, postpartum symptoms like this are not possible. They are, and no loss mother should feel ashamed to ask for help. The emotional and spiritual struggle following miscarriage does not always look like “depression;” it often manifests in anxiety, the inability to sleep, confusion or being overwhelmed, obsessive thoughts or extreme focus. Women experiencing these symptoms should seek medical attention. Mothers who have lost babies early in pregnancy should know that they are not alone, and that their grief may spread into many areas of their life. Women who have suffered losses previously can and should reach out to those miscarrying, helping them carry their burden and supporting them by working to address both their physical and emotional needs. Kathy Petersen is an RN and mother of 8 |
Archives
December 2023
Categories
All
|







 RSS Feed
RSS Feed